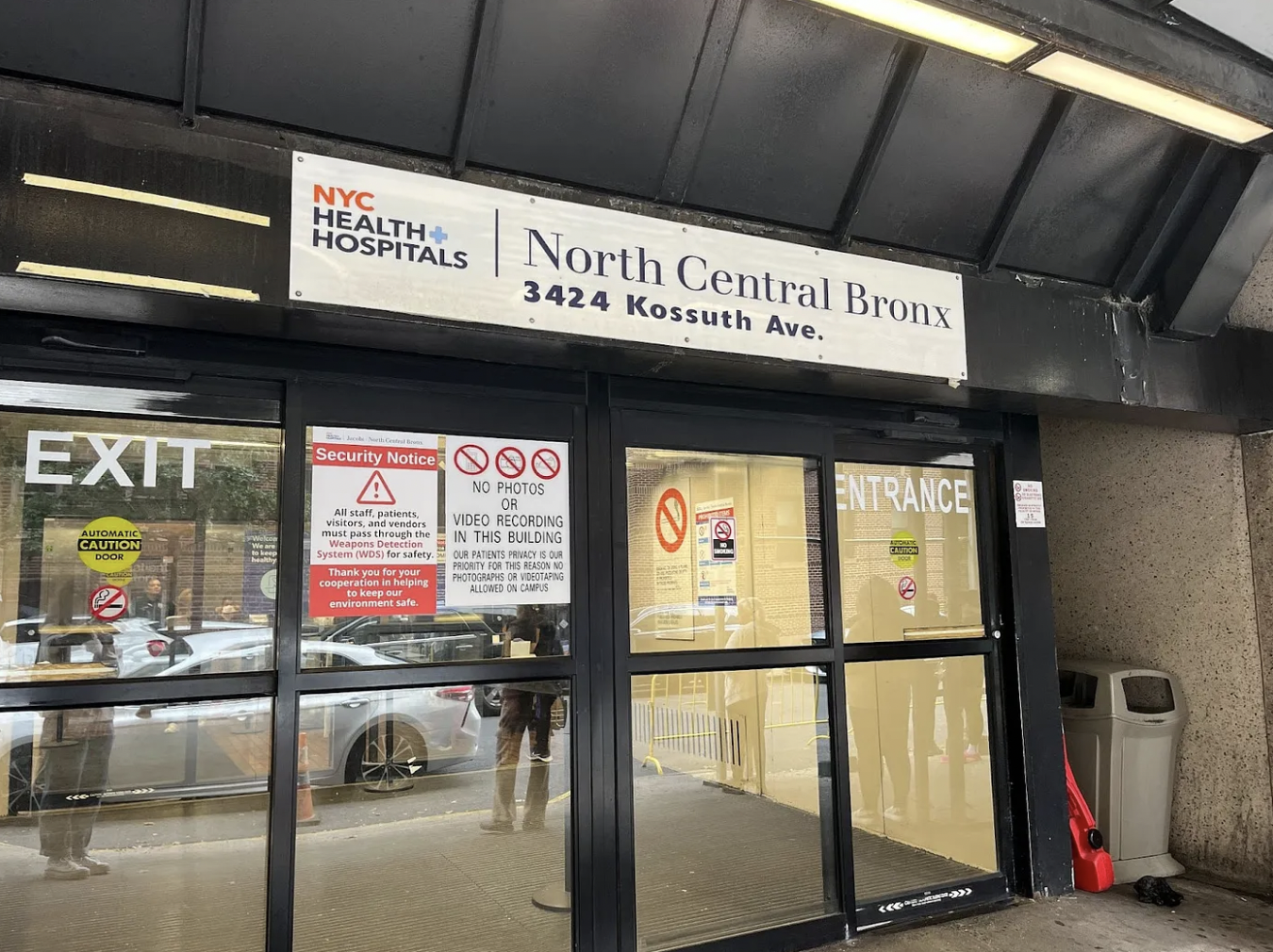
The entrance to NYC Health + Hospitals / North Central Bronx. (Credit: Julia Shannon-Grillo)
Most days, Nicolette Gressett begins her shift at North Central Bronx Hospital by 8 a.m. Along with one other midwife, she covers eight labor rooms and three triage rooms, in addition to daily postpartum rounds. She leads vaginal deliveries, assists in cesarean sections, conducts circumcisions, inserts birth control devices and even treats flu patients.
And for more than a year, Gressett has done this under an expired union contract.
“It’s demoralizing to have to continue, over and over again, to assert to your employer who you are and what you do,” Gressett said. “We have continued to go to work every day because not showing up would mean that the patients didn’t receive care.”
Gressett is a member of New York State Nurses Association (NYSNA), which represents licensed midwives at North Central Bronx and Jacobi hospitals. The two public institutions are “sister hospitals” within the NYC Health + Hospitals organization, meaning their midwives have been covered under one contract because some are credentialed to work at both facilities. On behalf of the midwives, the union contracts with Physician Affiliate Group of New York (PAGNY), a nonprofit group that provides services and personnel under an agreement with NYC Health + Hospitals.
But the midwives’ contract expired in July 2023. Since then, the union has been asking for a contract that would provide higher salaries, more midwives and longer visit times for patients whose first language is not English.
“We have had absolutely no success,” Gressett said.
NYSNA wants raises that would “bring their salaries up to what midwives are making at neighboring hospitals,” according to spokesperson Andrea Penman-Lomeli. Penman-Lomeli declined to share specific salary numbers. Current openings show that PAGNY is advertising a pay range of $120,000 to $150,000 for nurse-midwives at Jacobi.
The union also proposed that PAGNY hire two additional midwives at North Central Bronx and three midwives at Jacobi — requests that Penman-Lomeli said were rejected.
Representatives from PAGNY did not respond to multiple phone calls requesting comment.
Insurance companies have historically reimbursed hospitals at a lower rate for services provided by midwives than those provided by physicians. Two years ago, New York state increased their reimbursement rate to 95% of a physician’s rate for patients covered by Medicaid. Private insurers can still pay less, but state law requires them to cover some level of midwifery services.
Megan Fendt accepted a job as a licensed midwife at North Central Bronx in July, unaware that the contract had expired. If she had known beforehand, she said, she “wouldn’t have so readily accepted” the job. Now a few months in, she says current staffing levels have sparked concerns among staff for patient safety.
“If you’re not giving staff members what they need to keep themselves safe and for them to prioritize their own care for their own being, we can’t take care of other people,” Fendt said. “It feels really disrespectful.”
In 2020, amid continuing concern over maternal deaths, then-Bronx Borough President Ruben Diaz Jr. launched a task force whose members included administrators from both North Central Bronx and Jacobi. The following year, the Bronx had the highest number of maternal deaths by population in New York City, the most recent dataset available. That year, the task force made a series of recommendations, including the expansion of midwifery services.
But the practical results of their report remain unclear.
“I have shaken my fist into the sky when I think about the lack of changes since that report,” said Emily Slocum, a part-time midwife at North Central Bronx. “We are being asked to solve the maternity health care crisis in this country, and we’re not being given the resources.”
Slocum is also a lecturer at the University of Pennsylvania, where she teaches nursing and midwifery students. She said that inequities in maternal mortality have driven more research into the midwifery model, which is often correlated with better health outcomes for both the mother and child. It aims to minimize interventions to the natural birthing process.
A 2023 article by researchers at Yale School of Medicine found that midwifery care was associated with shorter hospital stays as well as fewer deaths, preterm births and C-sections. North Central Bronx and Jacobi hospitals have uniquely midwife-driven labor and delivery departments, according to Slocum. Obstetricians are called into vaginal deliveries only when complications arise. If a C-section is necessary, it is performed by an obstetrician.
One reason for the improved outcomes, the Yale researchers found, was that midwives often could conduct longer appointments than doctors could. The nurses’ union is asking PAGNY to extend visit times to ensure adequate care for patients whose first language is not English. Census data shows that 57.3% of Bronx residents speak a language other than English at home. The appointments often take longer, Fendt said, because midwives use a phone or video interpreting service for these patients.
“Anything related to visit timing or protection of time, PAGNY has said they have no control over,” because that is under the purview of NYC Health + Hospitals, Fendt said. “It’s a very weird punting of responsibility.”
NYC Health + Hospitals spokesperson Chris Miller declined to comment, writing in an email, “This is not our negotiation so there’s nothing else I can add here.”
Gressett blames some of the other delays in negotiations to turnover in PAGNY’s representation at the bargaining table. “They’re not up to speed on the negotiations when they show up. We basically are starting from square one every single meeting,” Gressett said.
The frustration has reached a breaking point for some. Following a negotiation meeting in July, Kaitlin Malone resigned from her role as a midwife at North Central Bronx.
“This will end somehow,” Malone said. “But at this point, I don’t see it ending soon or well.”
Malone accepted a new position as a midwife in a public hospital outside the state.
About the author(s)
Julia Shannon-Grillo, originally from Vermont, is a Stabile investigative fellow at Columbia Journalism School. Her reporting focuses on health care and public policy.